Is Testosterone Replacement Therapy Covered by Insurance?
If you’re considering testosterone replacement therapy (TRT) to treat low testosterone levels, one of the biggest questions is – will my insurance cover it? The costs of TRT can really add up between doctor visits, lab testing, medications, and more. Understanding your insurance benefits is crucial for accessing this treatment and managing expenses.
In this guide, we’ll break down everything you need to know about getting TRT covered by insurance.

Does Insurance Cover Testosterone Replacement Therapy (TRT)?
There’s no simple yes or no answer, as coverage varies based on your specific insurance plan. Some plans may cover TRT in full, while others have partial coverage or exclude it entirely. The best approach is to check directly with your insurance provider to get accurate, up-to-date information on your plan’s TRT coverage. It’s also wise to verify with your TRT provider that they accept your particular insurance.
Don’t get discouraged if coverage seems limited at first. Many plans cover TRT, especially when low testosterone is caused by an underlying medical condition and treatment is considered medically necessary. We’ll go over some key factors that can help increase your chances of coverage.
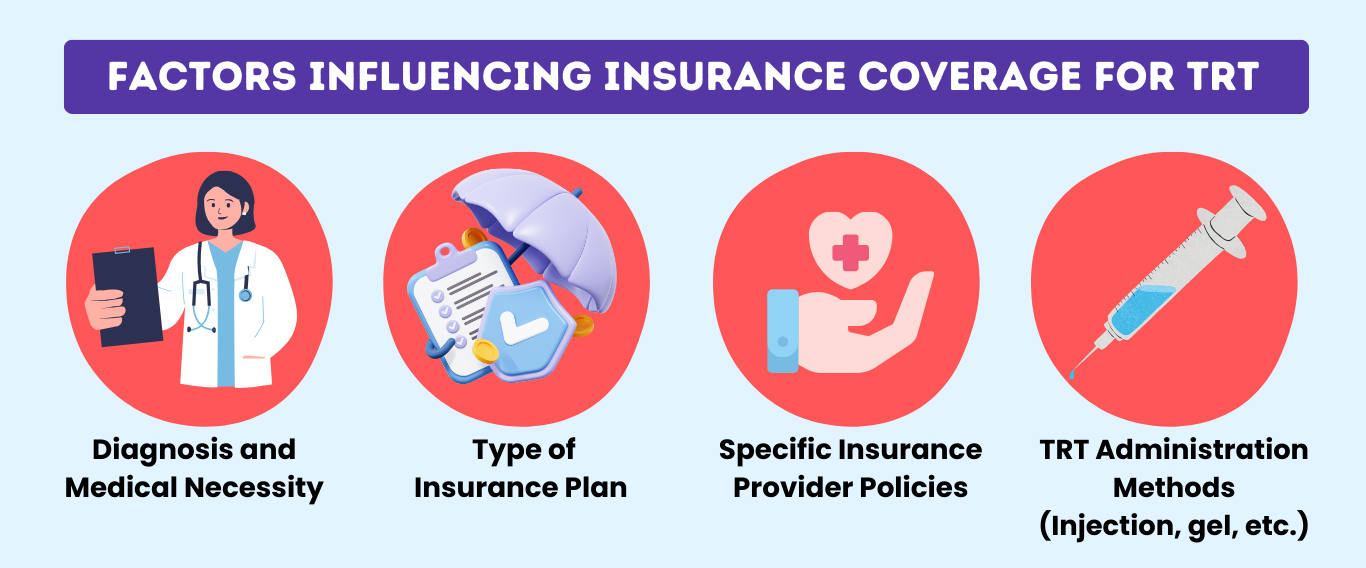
Factors Influencing Insurance Coverage for TRT
1. Diagnosis and Medical Necessity
Having a diagnosed medical condition that causes low testosterone, like hypogonadism, hypopituitarism, or pituitary disorders, greatly improves your odds of getting coverage for TRT. Insurers are much more likely to cover treatments considered medically necessary for treating a health condition.
Your healthcare provider will need to provide your diagnosis, lab results confirming low testosterone levels, and documentation that TRT is a medically necessary treatment for your specific condition. Building a strong medical case file is important.
2. Type of Insurance Plan
Coverage can differ significantly between private/employer insurance plans versus government plans like Medicare and Medicaid:
- Private Insurance: Policies vary by company and plan, with some being more willing to cover TRT than others. Employer-provided plans also have unique coverage rules.
- Medicare: Covers TRT when deemed medically necessary, but has strict qualifying criteria including very low testosterone levels. Medications may require high out-of-pocket costs.
- Medicaid: Coverage varies by state, but most state programs cover at least some formulations of TRT medications when medically necessary.
3. Specific Insurance Provider Policies
Each insurance company has their own internal coverage policies for TRT that evolved over time. For example, some insurers are more lenient in covering TRT for established medical conditions, while others restrict coverage to only the most severe cases of hypogonadism.
4. TRT Administration Methods (Injection, gel, etc.)
How you take your prescribed testosterone – injections, gels, pellets, patches, etc. – can impact coverage. Insurance providers often have preferences for certain delivery methods based on effectiveness data and costs. Your TRT medication must be administered in the covered way for the insurer to pay for it.
How to Determine If Your Insurance Covers TRT
Equipped with an understanding of the key factors, you can now take these steps to pinpoint your insurance coverage for TRT:
1. Review Your Insurance Policy Documents
Read through your detailed policy information carefully. Look for sections referencing hormone replacement therapy, testosterone therapy, or prescription drug coverage. Make note of any specific coverage rules, exclusions, limitations, pre-authorization requirements, etc.
2. Contact Your Insurance Provider for Clarification
After reviewing your written policy documents, you’ll still likely have outstanding questions.
This is when you’ll want to call or email a representative at your insurance company directly to:
- Verify if your plan covers TRT and get details on coverage rules
- Ask about criteria for coverage – diagnosis requirements, pre-approval, referrals, etc.
- Get clarification on covered TRT medications/delivery methods and dosage limits
- Understand costs – deductibles, copays, out-of-pocket maximums related to TRT
- Request a copy of the full coverage policy for TRT in writing
3. Questions to Ask Your Insurance Provider
When speaking to the insurance rep, get granular with your questions, such as:
- Does my plan cover testosterone replacement therapy for my specific diagnosis?
- What documentation/testing is required from my medical professional to justify medical necessity?
- Are all FDA-approved TRT medications and delivery methods like gels, injections, and pellets covered?
- Is there a preferred TRT medication or administration method that is covered?
- Do I need prior authorization or a special referral for TRT to be covered?
- Are there any annual caps, dosage limits, or duration limits on covered TRT treatment?
- Is there a separate deductible or higher copay/coinsurance for TRT medications?
Getting comprehensive answers will give you clarity on your TRT coverage situation.
Role of Your TRT Provider in Helping Determine Coverage
Your testosterone therapy provider or clinic is another key partner in navigating insurance benefits:
1. Assistance in Verifying TRT Insurance Coverage
Your TRT provider conducts lab reviews and consultations to determine if you’re a good candidate for therapy and assists in verifying your insurance coverage. They can reach out to your insurance on your behalf to verify coverage for your specific treatment plan. This includes supplying medical records justifying the need for TRT.
2. Guidance on Possible Out-of-Pocket Costs
Even if your TRT is partially covered, you may still face out-of-pocket expenses like deductibles, copays, coinsurance, etc. An experienced TRT provider can review your benefits and provide a close estimate of your potential costs based on your plan’s coverage details.
If costs seem unreasonably high, a good TRT clinic can explore alternative treatment options that may be more affordable with your insurance situation.

Amazing Meds: Your Partner in TRT Solutions
Our Approach to Online TRT
At Amazing Meds, we strive to increase access to TRT through online consultations and trusted telehealth services across the country. We understand navigating insurance for TRT treatments can be confusing and frustrating.
Our mission is to be a supportive partner throughout your TRT journey – including helping you fully understand and maximize your insurance coverage benefits:
- Dedicated staff to help verify if we accept your specific insurance plan for TRT
- Assistance obtaining documentation and pre-approvals to qualify for coverage
- Exploring treatment options to minimize out-of-pocket costs based on your benefits
- Providing affordable self-pay pricing for patients whose TRT is not covered
Contact Us Today About Insurance Acceptance
We’re just a call or message away to answer your questions about using your insurance for TRT with Amazing Meds. Taking that first step is easy!
Determining insurance coverage for TRT can seem overwhelming, but you don’t have to go it alone. With some guidance from your insurance and TRT provider, you can gain clarity on your benefits and treatment costs.
Starting TRT is a big decision – having affordable, high-quality care should be accessible to all men who need it.
Don’t let insurance confusion hold you back from exploring this potentially life-changing treatment. With some research and open communication with your provider and insurance, you can understand your options for affordable TRT.
TRT Insurance Coverage – A Visual Summary